Depressed Brain vs. Normal Brain: What Changes in the Brain During Depression?
- clytenjeri
- Jan 1
- 4 min read
Depression is far more than persistent sadness; it physically alters the brain’s structure and function in measurable ways. Understanding the differences between a normal, healthy brain and one affected by depression can clarify why the disorder impacts mood, cognition, and behavior so powerfully, and why effective treatment matters.
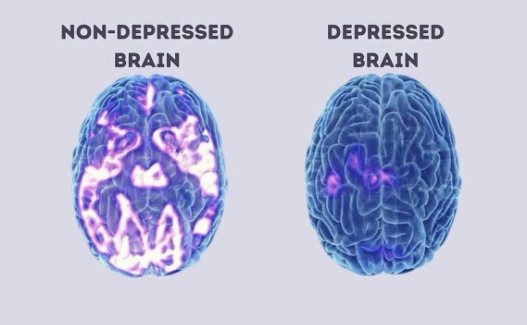
1. Neurological Differences: How Depression Reshapes the Brain
A. Structural Changes
Hippocampus Shrinkage. The hippocampus, essential for memory, learning, and emotional regulation, is often smaller in people with major depressive disorder compared to non-depressed individuals. This shrinkage is linked to chronic stress and elevated cortisol (the “stress hormone”), which impairs new neuron growth and weakens neural connections. Opel et al. (2014) observed in their study that reduced hippocampal volumes are frequently associated with Major Depressive Disorder, as seen in structural neuroimaging.
Prefrontal Cortex Abnormalities. The prefrontal cortex, responsible for decision-making, attention, planning, and impulse control, typically shows reduced activity and lower volume in the brains of individuals with depression. This can lead to difficulty concentrating, indecision, and emotional. Learn more
B. Functional Imbalances
Amygdala Hyperactivity. The amygdala, which processes emotion (especially fear and negative stimuli), tends to be overactive in depression. Depressed individuals show stronger amygdala responses to negative information, reinforcing negative memories and emotional sensitivity. Grogans, Fox & Shackman (2022) observed that amygdala hyperreactivity confers increased risk for MDD and other, often co-occurring internalizing illnesses
Altered Brain Wave Patterns: Brain electrical activity also differs; depressed individuals often exhibit increased alpha wave activity, which is associated with reduced responsiveness and cognitive engagement, compared to the balanced activity in healthy brains.
C. Neurochemical Imbalances
Neurotransmitter levels in depression are closely tied to imbalances in key neurotransmitters, chemical messengers such as serotonin, dopamine, and norepinephrine that regulate mood, motivation, and reward. Lower levels or disrupted signaling of these chemicals are commonly found in depressed brains and contribute to symptoms like low mood, lack of motivation, and anhedonia (loss of pleasure). Read more
2. The Impact of These Brain Differences
These neurological changes help explain why depression affects more than feelings; it disrupts cognitive function, emotional regulation, and even physical processes:
Memory and learning problems (hippocampus involvement)
Poor executive functioning (prefrontal cortex)
Persistent negative thought patterns (amygdala hyperactivity)
Motivational deficits and slowed thinking (neurotransmitter dysregulation)
Together, these changes create a cascade of symptoms that make daily functioning, work, relationships, and self-care significantly more challenging for individuals with depression.
3. Are These Brain Changes Permanent?
A critical question is whether depression causes irreversible brain damage, but research suggests many changes are potentially reversible.
For example, the hippocampal shrinkage associated with depression may be due not to the loss of neurons but to weakened dendrites. This means that recovery is possible, especially when treatments help restore synaptic health and reduce inflammation.
4. How Treatment Modalities Work to Restore the Depressed Brain
Effective treatment doesn’t just improve mood, it works at the neurobiological level to rebuild healthier brain function.
A. Medications
Antidepressants (like SSRIs and SNRIs) aim to correct neurotransmitter imbalances, improving communication between neurons. Over time, they can also boost neuroplasticity, the brain’s ability to form new connections, and help reduce inflammation associated with chronic depression.
B. Psychotherapy
Cognitive Behavioral Therapy (CBT) and similar therapies help reframe negative thinking patterns. These cognitive changes are accompanied by alterations in brain activity, particularly in the prefrontal cortex and amygdala, which reduce emotional reactivity and enhance executive control.
C. Lifestyle & Holistic Approaches
Exercise, meditation, and structured routines have all been shown to boost neurotransmitters and support brain health, thereby improving mood while reducing stress-induced cortisol levels. Some treatment programs also include creative therapies and social support, which enhance overall recovery.
5. Why Understanding the Brain Matters
The neurological perspective confirms that depression is a real brain-based disorder, not just “feeling sad.” Recognizing how depression alters brain structure and function helps:
✔ Reduce stigma
✔ Promote early intervention
✔ Support personalized treatment plans
✔ Inspire hope for recovery
With the right combination of therapy, medicine, and supportive care, many individuals can rebuild healthier brain function and lead meaningful lives.
How Jabali Health Helps Restore a Depressed Brain
At Jabali Health, we understand that depression isn’t just an emotional experience — it’s a neurological one. That’s why our approach focuses on supporting both the brain and the whole person.
1. Comprehensive Psychiatric Assessment
We look beyond symptoms. Through a detailed evaluation, we identify the biological, psychological, and lifestyle factors affecting your mental health. This allows us to create a treatment plan tailored to your brain’s unique needs.
2. Personalized Medication Management
When medication is appropriate, we start low, go slow, and monitor closely. Our goal is to correct neurotransmitter imbalances safely, minimizing side effects, and providing your brain with the stability it needs to heal.
3. Evidence-Based Therapy Options
We integrate therapies such as CBT and trauma-informed approaches that strengthen prefrontal regulation, reduce overactive amygdala responses, and help rewire negative thought patterns.
4. Holistic & Lifestyle Support
Because the brain responds to diet, sleep, movement, and stress levels, we incorporate:
nutritional guidance
sleep hygiene strategies
mind-body regulation skills
behavioral routines that rebuild structure and motivation
These interventions help lower cortisol, improve neuroplasticity, and support long-term recovery.
5. Continuous Follow-Up & Real Human Support
Healing takes time, and you don’t have to navigate it alone. We walk with you through every stage, adjusting your plan as your brain and body respond.
Depression is treatable, and early intervention leads to better outcomes.
Click here to schedule your session with Jabali Health to begin a personalized, evidence-based treatment plan.
REFERENCES
Grogans, S. E., Fox, A. S., & Shackman, A. J. (2022). The amygdala and depression: A sober reconsideration. American Journal of Psychiatry, 179(7), 454-457. https://doi.org/10.1176/appi.ajp.20220412
Opel, N., Redlich, R., Zwanzger, P., Grotegerd, D., Arolt, V., Heindel, W., Konrad, C., Kugel, H., & Dannlowski, U. (2014). Hippocampal atrophy in major depression: A function of childhood maltreatment rather than diagnosis? Neuropsychopharmacology, 39(12), 2723-2731. https://doi.org/10.1038/npp.2014.145
Pizzagalli, D. A., & Roberts, A. C. (2021). Correction: Prefrontal cortex and depression. Neuropsychopharmacology, 47(2), 609-609. https://doi.org/10.1038/s41386-021-01160-w
Schimelpfening. (2025, October 16). What is the chemistry behind depression? Verywell Mind. https://www.verywellmind.com/the-chemistry-of-depression-1065137
RELATED ARTICLES




Comments